Veiled
1
View details
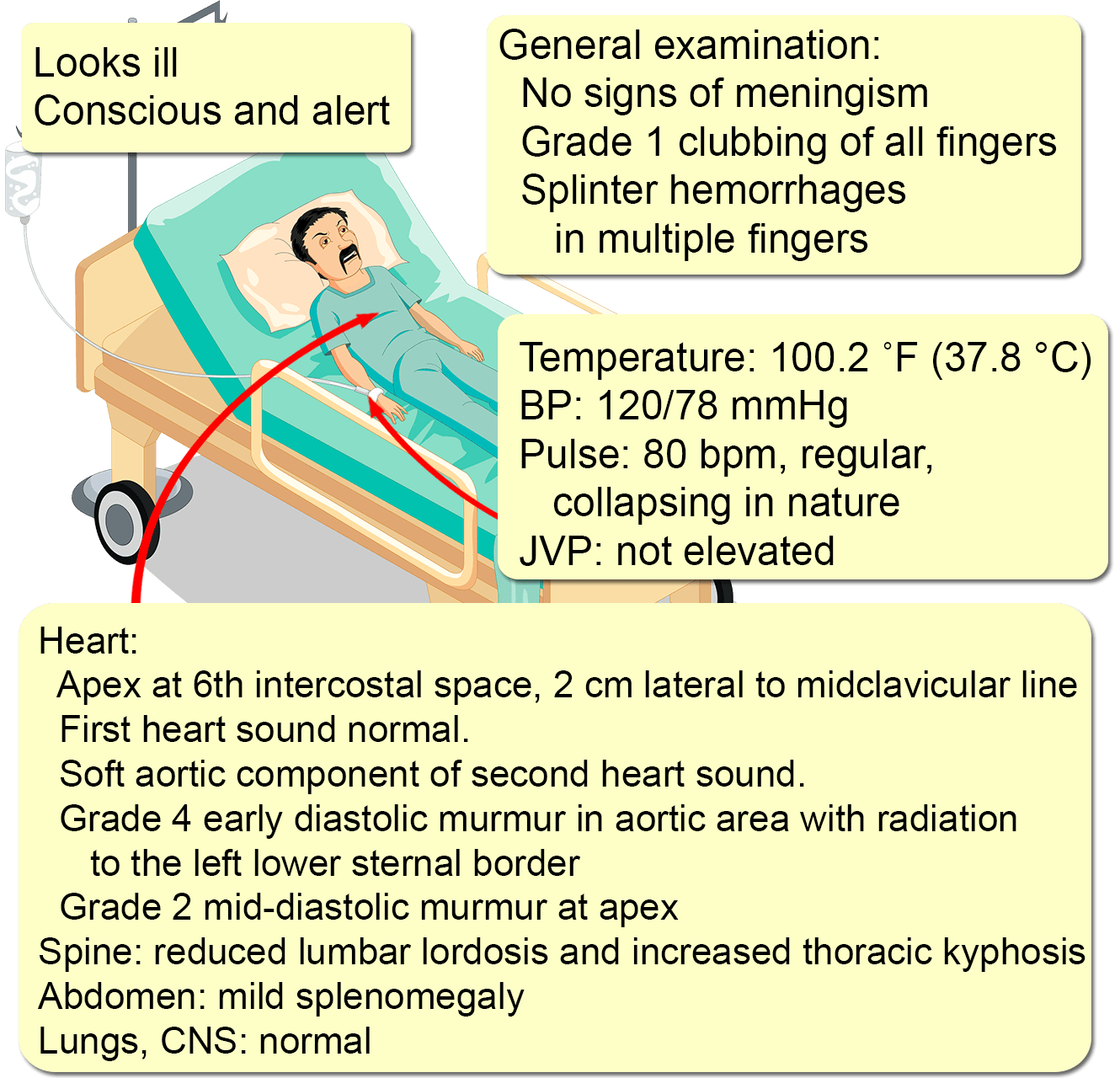
A 55-year-old man presents with a severe unremitting left-sided headache for two days that was of sudden onset. There is no history of photophobia, nausea, vomiting, numbness, weakness, visual disturbances, altered mentation, loss of consciousness, or recent head trauma. He has had an intermittent fever of up to 39 °C (102.2 °F) for two weeks, along with a 3 kg (6.6 pound) weight loss. No other symptoms were present.
His medical history is significant for ankylosing spondylitis for 30 years, complicated by aortic regurgitation for 20 years. He defaulted on his treatment 15 years ago and has not been followed up since. His surgical and family histories are unremarkable. He only drinks socially and does not smoke. There is no history of recent travel, or close contact with animals or sick individuals. Close questioning reveals a visit to a dentist three weeks ago, for scaling. He did not inform the dentist about his co-morbidities and did not receive antibiotic prophylaxis.
A full blood count is significant for a leukocyte count of 21,000/mm3 (normal: 4,500-11,000), with 85% neutrophils. His ESR is 102 mm/hour (normal: 0-22). Liver and renal functions are normal, as is a urinalysis. Chest x-rays show cardiomegaly. A noncontrast CT brain shows no mass lesions or features suggestive of focal or subarachnoid hemorrhage.